How Long Does Prednisolone Take to Work for Inflammation?
Understanding the timeline of how long prednisolone takes to work for inflammation can be crucial for managing various conditions treated with this effective corticosteroid. Prednisolone is often prescribed for its anti-inflammatory properties to alleviate symptoms associated with acute and chronic conditions. This article will delve into the mechanisms of prednisolone, its therapeutic effects, dosage recommendations, and what patients can expect regarding treatment duration.
The Mechanism of Action of Prednisolone
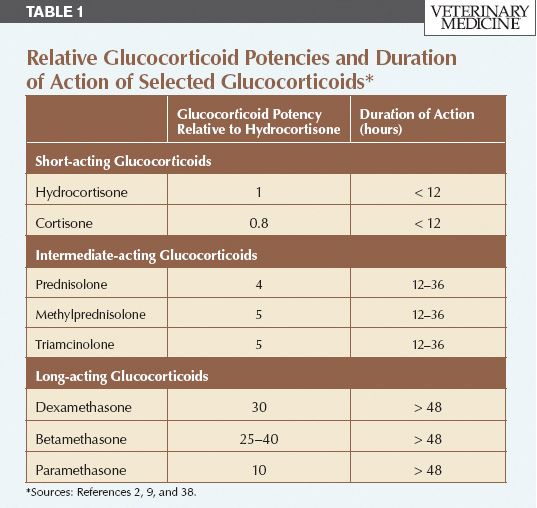
Prednisolone is a synthetic corticosteroid that mimics the body’s natural adrenal hormones. Its primary action is to suppress the immune response and inflammation, which is essential for managing conditions like arthritis, asthma, and other inflammatory diseases. When administered, prednisolone works at the cellular level to inhibit inflammatory pathways and immune response mechanisms, thereby reducing swelling and pain associated with inflammation. The onset of therapeutic effects can vary significantly, depending on the dosage and method of administration. Typically, patients may begin to notice improvements in their inflammation symptoms within a few hours to a few days after starting treatment, making timeliness a crucial aspect of prednisolone’s effectiveness.
Factors Affecting Prednisolone Onset
Several factors can influence how quickly prednisolone will demonstrate its effects. First, the **dosage** and administration route can play significant roles; higher doses and oral medication tend to work quickly for acute inflammation. Additionally, the individual’s health status and underlying conditions can impact the **immune response** to this corticosteroid. For instance, patients with chronic conditions like rheumatoid arthritis may experience a different response time compared to those dealing with acute inflammation. Moreover, prior treatments, like other anti-inflammatory medications, can influence **treatment response** and the overall effectiveness of prednisolone.
Understanding Dosage Recommendations
When prescribed prednisolone, it’s essential to adhere to the dosage recommendations provided by health professionals. Dosages typically vary based on factors including the circumstances of the inflammation, its severity, and the **duration of treatment** needed. In general, corticosteroids like prednisolone may start with a high initial dose, which may then be gradually **reduced**—this tapering schedule is crucial to avoid withdrawal symptoms or adrenal suppression. It’s vital for patients to avoid abrupt cessation unless directed by healthcare providers. Close monitoring of symptoms and response to treatment will guide health professionals in making necessary **dosage adjustments**.
Expected Timeline for Inflammation Relief
The timeline for observable effects of prednisolone varies depending on the type of inflammation being treated. Most patients can expect **symptom relief** relatively quickly when treating acute inflammatory conditions. Outcomes often range from a few hours up to days following initiation of treatment. For chronic conditions, however, it may take longer—sometimes, several days to a couple of weeks—for the full effects to manifest. Patients should be aware that while prednisolone can dramatically reduce symptoms during this time, it does not necessarily address the underlying cause of inflammation, necessitating a comprehensive treatment plan.
Understanding Treatment Duration
In terms of **treatment duration**, prednisolone is usually prescribed for the shortest time possible to mitigate the risk of side effects. Short-term use is common for acute inflamed injuries or flare-ups of chronic diseases. Health professionals often implement a strategic tapering plan after achieving control over inflammation to prevent potential adrenal suppression and rebound inflammation. Continuous or long-term low-dose therapy may be applied for chronic conditions, requiring **monitoring** to manage any side effects associated with prolonged corticosteroid use.
Monitoring Side Effects and Patient Responses
Monitoring for **side effects** is pertinent to enjoying the benefits of prednisolone therapy. Common side effects can include insomnia, weight gain, gastrointestinal disturbances, and increased susceptibility to infections. Patients should maintain open communication with their medical practitioners about symptoms experienced during treatment, which can inform whether a tapering schedule or dosage adjustment is needed. Health professionals often perform routine assessments to ensure medication compliance and effectiveness in managing inflammation while keeping an eye on contraindications and medication interactions.
Injection Versus Oral Prednisolone
When addressing how prednisolone is administered, there are crucial differences between oral medication and injectable forms. Oral prednisolone is widely used for inflammation management, providing adjustable dosages. However, in cases requiring rapid intervention—for instance, severe allergic reactions—injectable forms are often preferred as they typically yield faster therapeutic outcomes. Understanding the distinctions can significantly affect how healthcare providers design a patient’s **treatment plan**, balancing responsiveness against safety and side effects. Considering individual variability in response, health providers might opt for injections as a primary consideration during acute symptoms, followed by a transition to oral medications for long-term management.
Choosing the Right Administration Form
Deciding between injection versus oral prednisolone requires consideration of multiple factors, including the **current health status**, how quickly symptom relief is needed, and overall treatment goals. While oral corticosteroids are typically convenient for ongoing treatment, injections can effectively control serious, acute symptoms rapidly. Healthcare professionals assess each patient’s unique circumstances, including potential **drug interactions**, pre-existing conditions, and personal tolerance levels, to recommend the most suitable delivery form. Coordination between patient preferences and clinical guidelines assists in fostering effective **symptom management**, safeguarding against inefficiencies in the treatment strategy.
Impact on Long-Term Health Outcomes
Understanding the impact of long-term prednisolone use is also a pivotal aspect of management. Extended use of glucocorticoids like prednisolone can lead to complications such as adrenal suppression, and **health professionals** focus on minimizing such risks through appropriate tapering, regular dosage adjustments, and health monitoring. Studies underline the importance of developing comprehensive treatment guidelines that balance **immunosuppressant** effects with maintaining an optimal quality of life. Careful planning and communication between patients and providers become essential in ensuring that those on chronic corticosteroid therapy receive timely evaluations to safeguard their overall **health outcomes**.
Key Takeaways
- Prednisolone is effective for reducing inflammation, with a swift onset varying by dosage and administration type.
- Monitoring for side effects and patient responses is essential for optimizing treatment plans with corticosteroids.
- Both oral and injection administrations serve unique roles in managing inflammation, depending on patient’s needs.
- Long-term use requires careful oversight to minimize risks associated with glucocorticoid therapy.
FAQ
1. How quickly does prednisolone work for acute inflammation?
For acute inflammation, most patients experience a noticeable reduction in symptoms typically within hours to a few days after starting prednisolone. The swift response is due to the potent **anti-inflammatory** effects of this corticosteroid, which immediately targets inflammatory pathways.
2. Are there any side effects associated with long-term use of prednisolone?
Yes, long-term use of prednisolone can lead to various side effects, including weight gain, insulin resistance, adrenal suppression, and increased infection susceptibility. Regular **monitoring** by healthcare professionals is crucial to manage these risks effectively.
3. How is the dosage determined for prednisolone treatment?
The dosage of prednisolone is tailored based on several factors, including the severity of the inflammation, the patient’s overall health, past medication responses, and any underlying health conditions. Healthcare providers may initially begin with a higher dose that can be tapered as symptoms improve.
4. Can prednisolone be discontinued abruptly?
Discontinuing prednisolone abruptly is not advised, especially after prolonged use, as this may lead to withdrawal symptoms and worsening of the underlying condition. A gradual tapering plan should be followed, as outlined by a healthcare provider, to ensure a safe **treatment transition**.
5. How does prednisolone compare to prednisone for treating inflammation?
While prednisolone and its prodrug prednisone share similar therapeutic effects for inflammation, prednisolone is often more potent since it is already in its active form. This may lead to quicker **clinical outcomes** in certain inflammatory conditions.
Engaging in open discussions with healthcare professionals regarding treatment options and possible side effects empowers patients to manage their inflammation more effectively while navigating their ongoing health journey.